Inomyalgia: How to Navigate the Healthcare System
Inomyalgia: How to Navigate the Healthcare System
Inomyalgia may not be a widely recognized term, but for those living with it, the impact is profound. Characterized by persistent muscle pain, fatigue, and tenderness, this condition often leaves patients struggling for answers. Because it lacks clear diagnostic markers, navigating the healthcare system can be confusing and exhausting. Yet, with the right knowledge, advocacy, and support, individuals with inomyalgia can take meaningful steps toward relief and stability.
Understanding Inomyalgia
Inomyalgia is a chronic condition that primarily affects the muscles and soft tissues, leading to widespread pain and stiffness. Unlike injuries or localized pain disorders, inomyalgia symptoms often migrate or change in intensity, making diagnosis complex.
While research is still developing, experts believe a combination of genetic, environmental, and neurological factors contributes to the condition. Stress, infections, and hormonal changes may act as triggers. Because there is currently no definitive test, diagnosis often depends on symptom evaluation and ruling out similar conditions such as fibromyalgia or chronic fatigue syndrome.
Understanding inomyalgia begins with recognizing its complexity—both physically and emotionally. Patients frequently deal with anxiety, depression, and frustration alongside their pain, highlighting the importance of comprehensive, multidisciplinary care.
Common Symptoms and Misdiagnosis
The hallmark symptoms of inomyalgia include:
-
Persistent muscle pain and tenderness
-
Chronic fatigue despite adequate rest
-
Sleep disturbances and non-restorative sleep
-
Cognitive difficulties (“brain fog”)
-
Mood fluctuations or irritability
Because these symptoms overlap with other chronic pain conditions, many patients experience misdiagnosis. They may be told their pain is “psychological” or mistaken for other syndromes, which delays proper management. Recognizing symptom patterns early and tracking them in a health journal can be key to a more accurate diagnosis.
Diagnosis: What to Expect
There is currently no single test that confirms inomyalgia. Doctors typically perform:
-
Blood tests to rule out thyroid issues, autoimmune disorders, or infections
-
Physical exams to assess tender points or muscle response
-
Patient history reviews to identify patterns or triggers
Patients are encouraged to document their symptoms, noting onset, duration, and intensity. Bringing this information to appointments can help healthcare providers make more informed decisions.
Finding the Right Healthcare Provider
The right healthcare team can make a world of difference. Start by consulting rheumatologists, neurologists, or pain management specialists familiar with chronic musculoskeletal conditions.
Here are a few tips for choosing the right provider:
-
Ask about their experience treating inomyalgia or similar disorders.
-
Evaluate how well they listen and communicate during consultations.
-
Look for clinics that integrate physical therapy, mental health support, and lifestyle coaching.
If your provider dismisses your symptoms, don’t hesitate to seek a second opinion. You deserve a professional who treats your pain seriously and collaboratively.
The Power of Self-Advocacy
Self-advocacy isn’t just helpful—it’s essential. Educate yourself about inomyalgia and take an active role in your care. Here’s how:
-
Ask questions during appointments.
-
Request detailed explanations about medications or tests.
-
Bring someone with you to important consultations for support.
-
Keep a symptom tracker to discuss with your doctor.
When you voice your needs clearly, you help shape your treatment plan in meaningful ways.
Managing Inomyalgia: Treatments and Strategies
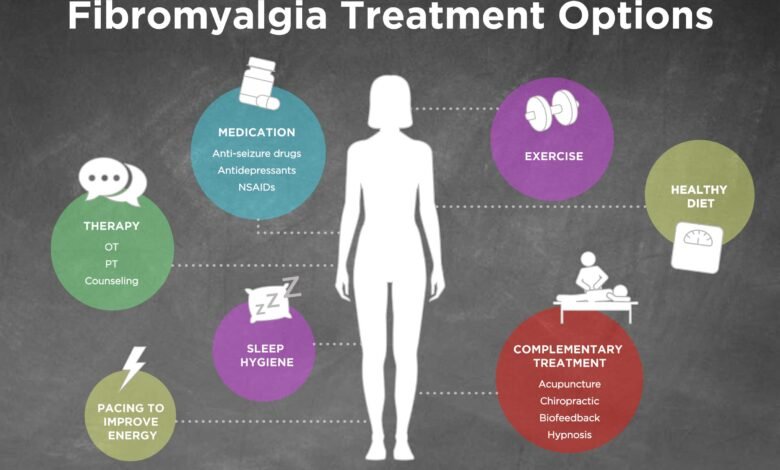
Managing inomyalgia often requires a multifaceted approach. No single treatment works for everyone, but combining medical, physical, and mental strategies can offer relief.
1. Medical Treatments
-
Pain relievers (NSAIDs) for muscle pain and inflammation.
-
Antidepressants or anticonvulsants to manage chronic pain signaling.
-
Sleep aids to improve rest quality.
2. Physical & Lifestyle Therapies
-
Gentle exercises such as stretching, yoga, or swimming.
-
Balanced nutrition with anti-inflammatory foods (omega-3s, leafy greens, turmeric).
-
Consistent sleep routines to enhance recovery.
-
Stress reduction through mindfulness or deep-breathing techniques.
3. Alternative and Complementary Options
Some patients find relief through acupuncture, massage therapy, chiropractic care, or biofeedback. These should complement—not replace—conventional treatments.
Coping and Support Systems
Emotional well-being is equally vital. Consider building a support network that includes:
-
Support groups (local or online) for shared experiences and coping tips.
-
Family and friends, once educated about your condition.
-
Mental health professionals specializing in chronic pain or anxiety.
Community can make an enormous difference when facing an invisible illness.
Living with Inomyalgia: Long-Term Outlook
While there is no known cure, many individuals successfully manage inomyalgia through consistent self-care and medical guidance. Over time, understanding your triggers and responses helps reduce flare-ups and improve quality of life.
Patience, persistence, and self-compassion are key. Small, consistent adjustments often lead to long-term improvement.
FAQs About Inomyalgia
1. Is inomyalgia the same as fibromyalgia?
Not exactly. While both share similar symptoms, inomyalgia may have distinct biological markers and could represent a broader spectrum of muscle pain disorders still being studied.
2. Can inomyalgia be cured?
Currently, there’s no cure, but symptoms can be managed effectively through a combination of therapies and lifestyle changes.
3. What triggers flare-ups?
Common triggers include stress, overexertion, lack of sleep, hormonal shifts, and poor diet.
4. How can I support someone with inomyalgia?
Listen, believe their pain, and offer practical help—like assisting with chores or accompanying them to appointments.
Conclusion
Navigating the healthcare system with inomyalgia can be daunting, but knowledge and self-advocacy make all the difference. With the right provider, treatment plan, and support network, it’s possible to reclaim comfort and control over your life. You are not alone—understanding, persistence, and community are powerful allies on your path to healing.




